Analyzing Cells to Better Understand FASD
Project Category: Projects – Cycle II
March 21, 2021
Challenge
The ability to better characterize the cellular mechanisms underlying brain dysfunction in FASD is vital to treat the disorder better. The purpose of this project is to provide a detailed understanding of these mechanisms as a means of possibly identifying novel targets for future drug development.
Project Summary
Studies have shown that prenatal alcohol exposure (PAE) leads to an increased likelihood of developing seizures. There is a good chance the hippocampus is the brain region responsible for this phenomenon. Hence, a team led by Dr. Peter Carlen (University Health Network in Toronto) studied this brain structure in young mice with PAE. They found the cells in these mice displayed hyperexcitability, which could account for increased seizure susceptibility in FASD.
The team also discovered that in FASD mouse models, the blood-brain barrier—a filtering mechanism that carries blood to the brain and is responsible for blocking the passage of certain substances—was leaky. The team is testing novel therapeutics to repair the blood-brain barrier.
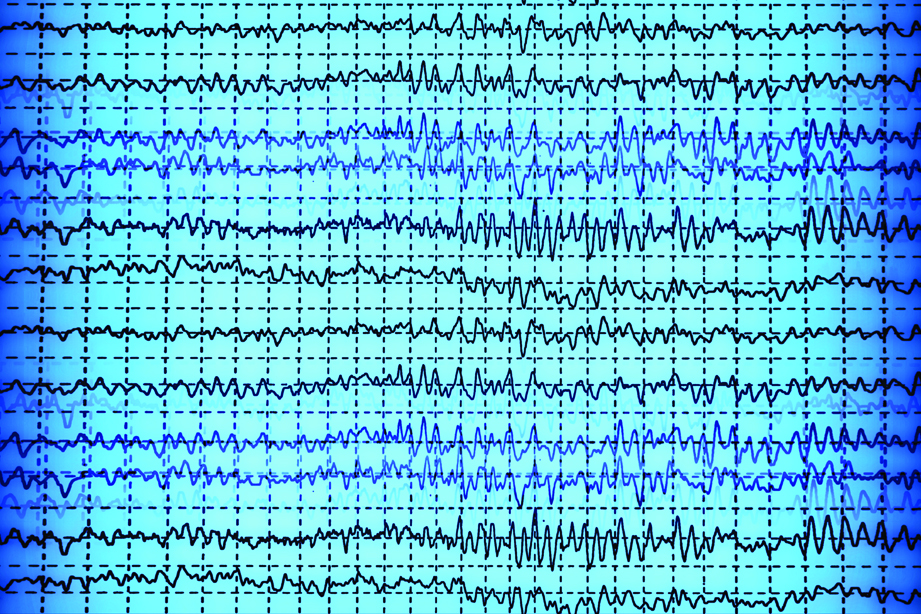
Researchers have established a guinea pig model of FASD to do electroencephalogram
(EEG) scans on the animals while they are awake. Preliminary results show similarities with the mouse model—the cells in the brain become hyperexcitable in guinea pigs with PAE, which could potentially be a cerebral biomarker for PAE. The team is testing anticonvulsants—currently used to treat epileptic seizures—in guinea pigs with PAE to see if it reverses any of their symptoms.
Result
The project has led to a collaboration with Dr. Geog Zoidl (York University) to analyze further cellular mechanisms involved in FASD. Preliminary evidence suggests molecular changes in the brain associated with PAE are a result of a deficient blood-brain barrier. This deficiency, in turn, compromises astrocytic cell function and causes demyelination. Astrocytes are the most numerous cell type in the central nervous system and perform many essential tasks. Demyelination occurs when the protective coating of the nerve cells are damaged, resulting in neurological challenges.
Funding
This subproject was part of the larger “FASD: Early Life Adversity, Outcomes and Secondary Intervention and Prevention.” The FASD program was funded a total of $1,205,381 from the Kids Brain Health Network and $2,148,667 from participating partners.
Team
Dr. Peter Carlen, University Health Network in Toronto